Mixing Covid-19 vaccines has been tried out of necessity in some countries because the supply of a particular vaccine ran short. However, the “heterologous prime-boost” approach is not a new idea and makes a lot of sense biologically.
Scientists have long theorized that giving people two slightly different vaccines might generate a stronger immune response, which has been tested in fighting other diseases including Ebola. Each vaccine may teach the immune system to recognize different parts of a virus or may stimulate slightly different parts of the immune system, resulting in broader protection. The Sputnik V Covid-19 vaccine already uses the general principle of prime boost with two different viral vectors.
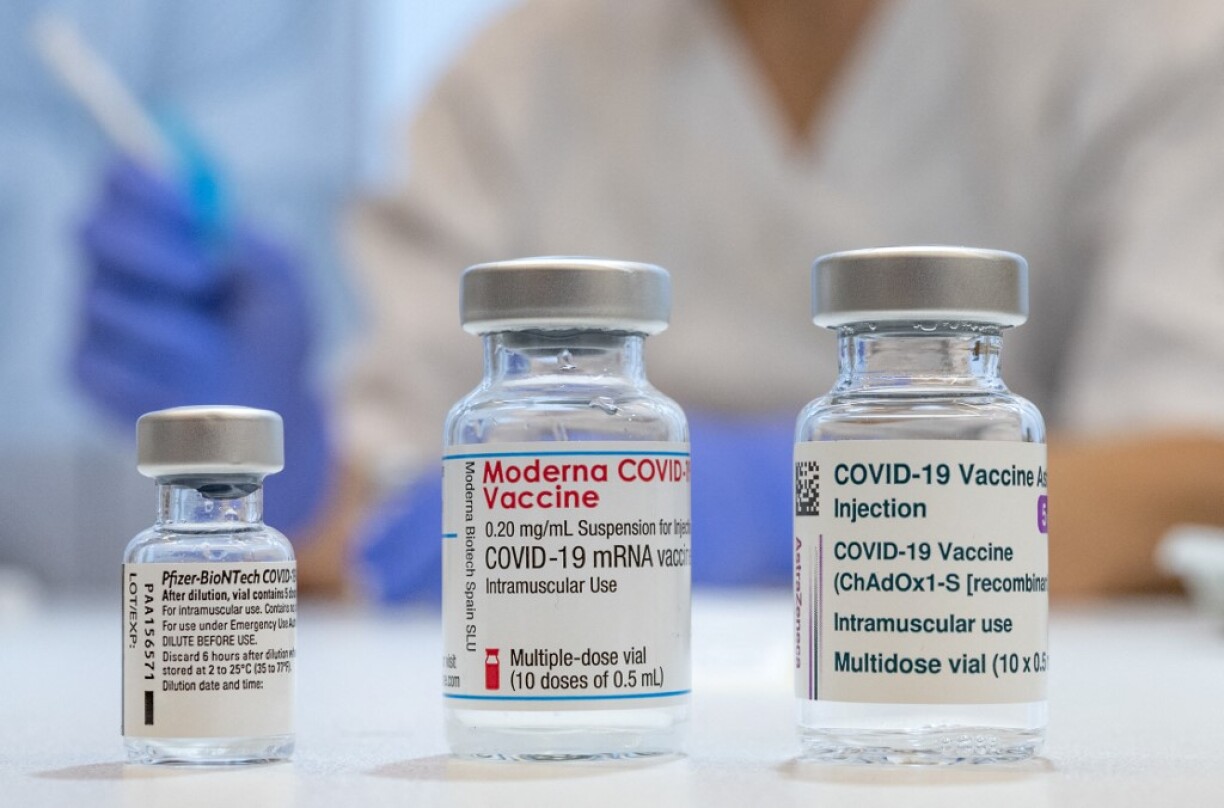
The Oxford–AstraZeneca vaccine uses a harmless virus (adenovirus) to carry genetic material from SARS-CoV-2 into cells. This technology mimics what happens during natural infection and has a good track record of inducing strong T-cell responses. Immunity levels build over time and stretching the dosing period seems to increase protection. On the other hand, vaccines using the mRNA technology, like Pfizer–BioNTech and Moderna, have been shown to elicit exceptionally good antibody responses. Mixing these two technologies may therefore provide the best of two worlds.
Mixing the Oxford–AstraZeneca and Pfizer–BioNTech COVID-19 vaccines appears to produce a potent immune response against SARS-CoV-2. Early results from two independent studies from Spain and the UK with 676 and 830 people respectively report that giving people Pfizer–BioNTech, after receiving a first dose of the Oxford–AstraZeneca vaccine, results in high levels of neutralizing antibodies. Neutralizing antibodies are probably a good indicator for predicting efficacy because they help prevent viral infection, but T cells are thought to protect against severe disease by killing cells that have already been infected.
In the UK study, also known as the Com-COV study, the highest antibody response was found in people who received the standard two shots of Pfizer–BioNTech. However, the response was almost as high in the combination of Oxford–AstraZeneca followed by Pfizer–BioNTech. This combination also had the best T-cell response, which was more than double that from the two Pfizer–BioNTech doses. These results are supported by another study from Germany, which reports that this mixed approach was better at activating an immune response than the standard two Oxford–AstraZeneca vaccines.
Notably, the data from mixed vaccine trials do not necessary mean that two doses of Oxford–AstraZeneca are somehow inferior. It is worth noting that two doses of the Oxford–AstraZeneca vaccine has already proven to be highly effective, reducing hospitalisations by more than 90%. Indeed, these preliminary publications are pre-prints - meaning that they have not yet been peer-reviewed.
There are other limitations to be aware of when interpreting the results from the available data, including the small number of participants in studies and different intervals between doses that make it difficult to pick up any rare side effects. This is leading some researchers to recommend sticking to the standard two shots of a single vaccine for now, which has proven to be both safe and effective in the real world.
But with the arrival of new SARS-Cov-2 variants, the results from mixed vaccine trials could be important in finding the most protective combinations. It will also help prevent stalling of vaccine roll out when supplies are low.
Understanding more about the subtle differences in the immune response activated by each vaccine, and how they could be mixed, could also lead to individualized strategies. For example, combinations that result in good T-cell responses may become a better option for people who are taking medication to suppress their immune systems, and therefore often cannot create strong antibody responses.
The Com-COV study has already begun testing other vaccines including the yet-to-be-approved protein-based vaccine developed by the pharmaceutical company Novavax. A study in the US has also started testing the mixed vaccine approach with Johnson & Johnson, which only requires one dose as standard today.
Mixing Covid jabs has good immune response, study finds
Safety and Immunogenicity Report from the Com-COV Study
Mixed Oxford/Pfizer vaccine schedules generate robust immune response against COVID-19
Mix-and-match COVID vaccines: the case is growing, but questions remain
Why More People Are Getting Two Different Coronavirus Vaccines
Sputnik V COVID-19 vaccine candidate appears safe and effective
Safety and Immunogenicity Report from the Com-COV Study
Safety, reactogenicity, and immunogenicity of homologous and heterologous prime-boost immunisation with ChAdOx1-nCoV19 and BNT162b2
Immunogenicity and reactogenicity of a heterologous COVID-19 prime-boost vaccination compared with homologous vaccine regimens
Reactogenicity and Immunogenicity of BNT162b2 in Subjects Having Received a First Dose of ChAdOx1s