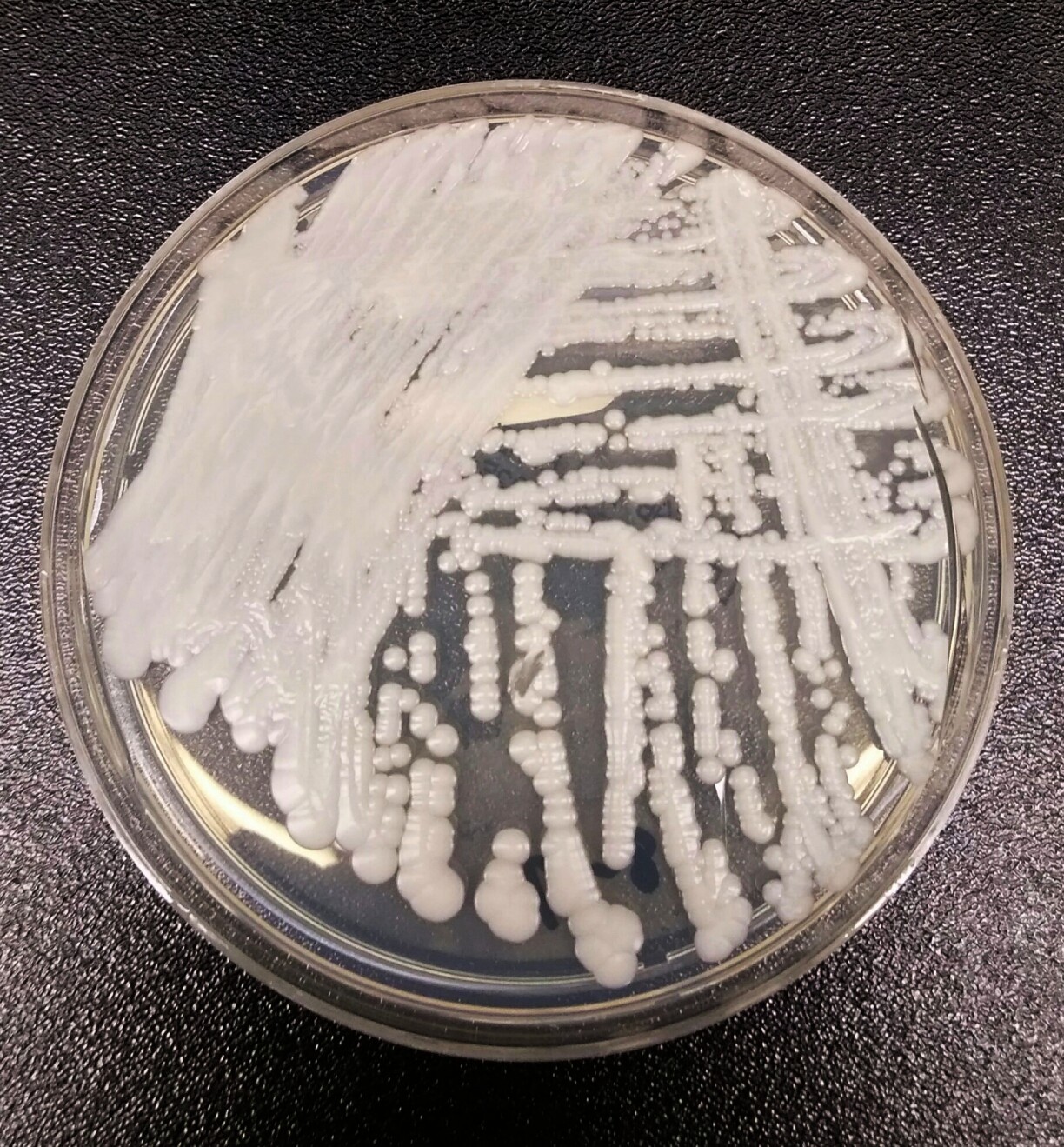
Candida auris infections have skyrocketed across Europe, with cases rising from 804 to 1,346 between 2022 and 2023 alone. The pathogenic yeast – which carries an estimated mortality rate ranging from 29% and 62% – was first reported on EU territory in 2014 and has continued to spread ever since.
Neighbouring countries Germany, France, and Belgium reported 77, 10 and six cases respectively in 2023, and just this week, Tagesspiegel reported Germany’s second-biggest outbreak at Berlin’s Charité hospital and German media are warning of its dangers.
Despite increasing infection numbers, the European Centre for Disease Prevention and Control (ECDC) recently reported that many countries still show gaps in national preparedness regarding surveillance, infection, and control measures.
We reached out to the Ministry of Health to get a scope on the situation in the Grand-Duchy.
In their reply, the Health Directorate of the Ministry stated that the danger of Candida auris has not been ignored in the Grand Duchy. They explained that measures such as mandatory case notification and a national surveillance system have already been implemented, and assured that Luxembourgish laboratories are able to detect the pathogen if necessary.
However, the ECDC reported that Luxembourg still lacks specific guidance on laboratory testing, clinical management, and infection control, while neighbouring countries such as Germany and Belgium have already adopted such measures.
The Directorate emphasised that in the event of an outbreak, hospitals, and laboratories could rely on recommendations from neighbouring countries or at the European level. “Hospital infection prevention and control teams are familiar with the precautions required for this type of infection and can implement them properly”, it noted, adding that even without national guidelines, “hospitals would promptly implement the standard measures known to control Candida auris.”
Finally, the Directorate highlighted Luxembourg’s small size as an advantage, as it would allow authorities “to quickly mobilise all key players as soon as a case is detected, which is an advantage in containing a potential emerging epidemic”.
While there’s no reported cases in Luxembourg, most infection or colonisation cases in Europe have been reported in healthcare facilities.
According to the Health Directorate, treatment is particularly complicated, they explain that the yeast’s capacity to rapidly develop resistance to drugs “complicates its treatment and prolongs the period during which a patient remains a carrier”, raising therefore the risk of transmission.
What makes it stand out, is its ability to survive otherwise hostile conditions, the Directorate explained. “It can also persist for long periods in the environment, particularly on inert materials, and has the ability to adapt to high temperatures or high salt concentrations,” underlining that these characteristics are partially responsible for the rise of outbreaks in hospitals.
According to the Directorate, the most severe cases were observed in immunocompromised individuals, for example patients undergoing chemotherapy or those hospitalised in intensive care.
They explain that Candida auris, unlike other species of the same group, is not part of the normal human flora, meaning that to cause harm or spread, it has to colonise an individual, often on the skin. This can occur in hospitals where the fungus is present.
“Candida auris can persist for long periods on dry or wet surfaces, as well as on inanimate objects”, the Directorate stated, underlining that it can live and spread through colonised or infected patients and in infected environments. It can be transmitted from person to person, or via contaminated objects like medical devices and surfaces.
The US’s Centres for Disease Control and Prevention (CDC) state that the contagious fungus can cause infections in different parts of the body, for example in wounds, blood, or the ears. They note that there’s no specific set of symptoms for Candida auris, but symptoms can resemble those found in bacterial infections, such as fever or chills.
It’s important to note that people carrying the fungus can be asymptomatic. The UK’s National Health Service (NHS) states that Candida auris is particularly dangerous for hospitalised patients, as it can enter the body during medical treatments or surgical wounds. This may occur during operations or when inserting devices such as drips or urinary catheters.
When it comes to prevention, the NHS emphasises the importance of hand hygiene for hospital workers and visitors dealing with infected patients. Hands should be washed before and after every contact with patients, and alcohol-based hand gel should also be used. It is important to avoid touching wounds or broken skin.